The patient-physician relationship is the cornerstone of healthcare, and it is based on mutual respect, trust, and open communication. Patients need to be able to trust their physician to provide high quality care while maintaining confidentiality and protecting the patient’s sensitive medical information. Effective communication is essential to understand and address patients’ questions and concerns, while involving the patient fully in the decision-making process.
Physicians must obtain informed consent from each patient when initiating any treatment or course of action, allowing the patient to make an educated and autonomous choice about his/her healthcare. This is a critical ethical and legal concept: the patient should be fully informed about potential risks, benefits, and alternatives of the medical treatment before making a decision.
Physicians should always respect their patients’ right to make informed decisions about their own healthcare, based on their own values and preferences. This includes the right to accept or refuse a particular course of action. Physicians should always respect the patient’s wishes, even when the physician disagrees with those wishes.
One of the most important principles in medicine is “First, Do No Harm”, or Primum Non Nocere. The physician should avoid any action that could cause harm to the patient, and should serve as an advocate for their patient, working in their best interest to ensure the best possible outcome.
What Happened in Early 2020?
- A virus
- Fear propaganda
- Lockdowns
- Mandates
- Censorship
- Persecution
How Did the Pandemic Affect the Patient-Physician Relationship?
These past three years exposed the weaknesses in the patient-physician relationship. The mask mandates, lockdowns, travel restrictions and vaccine mandates, just to name a few – which were all endorsed by the CDC, medical organizations, and healthcare institutions – in many cases interfered directly with the patient-physician relationship.
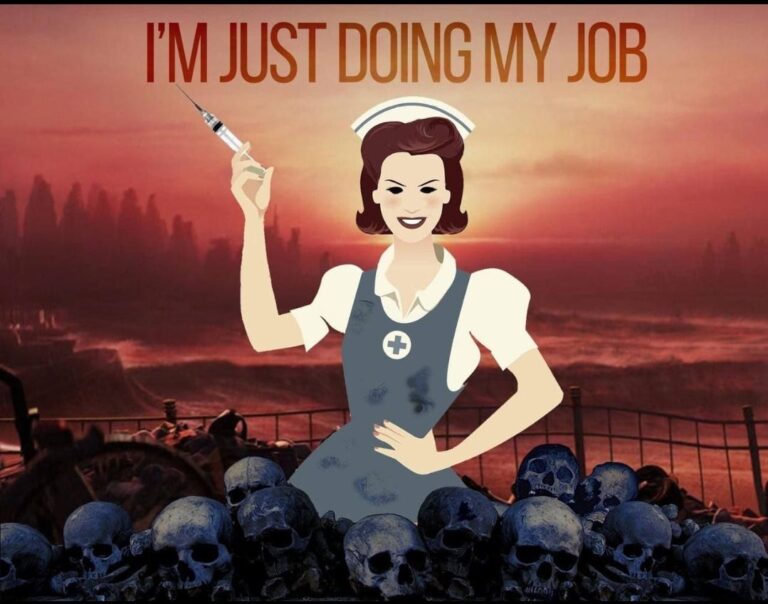
The environment of outright censorship of science and persecution of physicians who spoke against the mainstream narrative left many physicians unwilling to swim against the current. While the institutions and the system mandated certain procedures and actions to be followed uniformly, many patients disagreed, and patients felt abandoned by their physicians. In some cases where the patient and physician disagreed on a specific course of action, physicians refused to comply with patient wishes and offered only ‘one size fits all’ medicine. Based on everything we know in medicine, this was a complete breach of trust.
Now we are facing the fallout from the behavior of the healthcare system during the pandemic, and we find ourselves navigating rough waters. If there is no trust left, is there even a patient-physician relationship?
What Does the Future Hold?
The trust once broken will take a while to rebuild; there is no doubt about that. It starts with physicians and our commitment to the Hippocratic Oath, those sacred words of “First, Do No Harm”. The practice of medicine has been corrupted for years, through big pharma, regulatory decisions, the corporate practice of medicine and in some instances, government-run healthcare.
The true art of medicine is and always has been keeping the health and well-being of the patient as the primary focus. That focus was lost along the way. Healthcare has become the business of illness and not health. We must return to the basics. As Thomas Edison once said: “The doctors of the future will give no medicine but will interest his patients in the care of the human frame, in diet and in cause and prevention of disease.”
The Dangers Ahead
The World Health Organization (WHO) is currently working on two different approaches to how pandemics will be managed in the future: a new Pandemic Treaty, and amendments to the existing International Health Regulations. Both are an attempt to strengthen the WHO’s control over future pandemic responses. Under the treaty and new amendments, the WHO would focus on:
- early detection and prevention of future pandemics
- universal and equitable responses for all with vaccines, medicines and diagnostics
- a stronger international health framework with WHO in charge
- the “ONE HEALTH” approach, that would connect the health of humans, animals, and the planet
As such, the patient-physician relationship as we know it would further erode. While until recently physicians advocated and “worked” for the patient, with WHO mandates in place, the physician would have to comply with them and follow the directives of the system.
The question that remains is, will physicians recognize the perils of such actions or will they continue on the path of patient abandonment? Time will tell.
“To be courageous requires no exceptional qualifications, no magic formula, no special combination of time, place, and circumstance. It is an opportunity that sooner or later is presented to us all.” John F. Kennedy